“I’ll never go on antidepressants. Once you start, how do you stop?” —a friend
A couple of weeks ago I paid my biannual visit to the Manhattan office of the woman who prescribes me my medication. For many years I have been on two classes of medication: a selective serotonin re-uptake inhibitor (first Effexor, now Lexapro), and a benzodiazepine, typically Ativan, which I take only at times of acute distress. The woman who prescribes my medication is a psychiatric nurse. She does not provide therapeutic services and she does not have a medical degree. From what I have gathered, she spent much of her career working on an impatient psychiatric ward. She charges $140 an hour, which, given the relief she provides, is a very reasonable expense. For years she was a heavy smoker; the habit has done lovely things to her voice.
Like a lot of anxious people, particularly, I suspect, those of the bookish, cerebral type, I have an actively conflicted relationship with my medications (or, I should probably say, with the fact of my being medicated). On the one hand, as I say, the pills provide relief — although in this claim, I see, already lies the seed of the conflict, for I can not be certain that the pills provide relief. The Ativan is exempt from the dilemma: it has a quick and discernible sedative effect. A benzodiazepine, the best known brands of which are Ativan and Xanax, acts like a martini, but without the inebriation. The problem pill is the SSRI, the efficacy of which can be very hard to gauge. How can you be sure it’s working? Anxiety, like all psychiatric complaints, is subjective. Despite the best efforts of the clinical establishment, the only extant measures of anxiety are purely linguistic: answers to the old eye-roller, “How are you feeling?” There is no blood test, no objective factor like blood sugar or cancer markers. There is only the blooming, buzzing, oceanic flux of experience: description.
At first, if my experience is any guide, the matter of medication efficacy isn’t terribly fraught. When an anxious person first goes on an SSRI, she typically does so because she is in crisis, and the medication either works or it doesn’t. Let six weeks pass. Is there still a crisis? Then the medication isn’t working. Has the crisis abated? Then the medication is working. There remains some doubt clouding the picture, because usually the patient is simultaneously in talk therapy, which could conceivably be the dominant clinical factor. But we are talking here of crises — pronounced and atrocious spikes in mood. Therapy works more slowly than pills. A person can simply tell.
As time goes on, however, and the spike does not recur, and one keeps ingesting the pills and, with a dutiful self-preservation, keeps talking to one’s shrink and making responsible adjustments in one’s habits — in diet, in exercise, in romance, in work —a more serious and insidious confusion creeps in. Changes have been made, real changes. The anxiety is there — it will always be there; you admit this to yourself — but it is now, as the clinicians say, “manageable.” To what do you one owe this protracted, if incomplete, relief: medication or will? Once you needed the pills — urgently you needed the pills. But do you still need the pills? How can you be sure they’re even still working? If the pills were discontinued would the panic come raging and roaring back? Or would life continue along as it is now? Doesn’t it make sense — wouldn’t it make perfect sense — to wean yourself from the medication, to see if it is no longer essential to your continued contented existence?
It does make sense. This is how the medication was sold to you, after all — as a temporary measure, something to get you over the hump. It is troubling, then when you resolve to thank this natural step and you are assailed, quickly, by two vexing and countervailing questions. The first question regards timing. Wisely, you want to be sure that you are not going off your medication during a period of transition or flux in your life. You do not want to be reckless. And yet you know well (because like many anxious people you have looked into Buddhism and absorbed its precepts) that life is nothing but transition and flux — transition and flux to which, you also know well, you are prone by virtue of your anxious temperament to respond with painfully exquisite sensitivity. Now is not the right time. This is the boldness-killing thought. Just now I have an assignment to finish. Just now my child is entering school. Just not my wife and I are quarreling. Just now we are about to move. Just now. Just now I want to be sure of my sanity.
The second question to enter your mind is: Why bother? For me, at least, SSRIs have never caused a significant side effect. I don’t experience constipation, diarrhea, dizziness, drowsiness, dry mouth, headaches, light-headedness, loss of appetite, or nausea. I can still easily summon an erection and I can still reach orgasm. The only annoyance is the very mild one of being handcuffed to the pills themselves: it’s one more thing to before bed, along with brushing my teeth and removing my contact lenses; it’s one more item to remember to pack in my carry-on luggage. There is still, it’s true, the nagging stigma of being among the medicated — but at a time when twenty percent of Americans are on some kind of psychiatric drug, whatever shame one feels is very arguably self-imposed and anachronistic. You’re on a pill. So what? What’s the big deal? May as well continue along as before…..
And so it is that every six months or so I take the subway to the West Side, ascend to the seventh floor of a tall, beige-stone building, and sit thumbing through a Vanity Fair with a check in my pocket, waiting for a fresh prescription. It has been — I don’t know exactly how long it has been. Six years? Eight? Ten? A long time. Periodically I ask the woman who prescribes me my pills how I might go about getting off them. I defer to her expertise — nervously, I defer. Is it a good idea? Is now a good time? She is a person who prescribes medication for a living. She is, in other words, a true believer. But she is ethical and understanding as well, and she tells me that “we” can try. Here is how we might go about it. Here is a schedule, a method, whereby we can lower the dosage — slowly, slowly, until the pills are no more.
I carefully write these instructions down. I always write these instructions down. But I have yet to use them, or even to start the process.
Starting is, of course, the vital step.






You don’t need the pills. The economy needs your money.
Yeah, you’re right.
Ugh.
This is a very good description of the mental process when trying to free oneself from medication. I have tried to go off my meds at least 4 times, always with the “I think I can deal with life now” attitude. I do fine for up to 6 months, then, my world comes crashing down again and I am just trying to survive. I grudgingly go back on the meds, slowly get better, then vow that I will not try THAT again… until a few years later, when I say to myself “I think I can deal with life now”.
I would say this: Anti depressants may have long term negative effects-the research is usually no longer than a year so that would concern me-
another thing the research does not show a very robust effect compared to placebo and it has been argued by some that the side effects are what give the ssri’s an edge over placebo-the patient suffers a side effect and concludes he is on the real thing-hence placebo effect strenghthened.
I experimented with lexapro 10 mg severasl times after being on it for one year-went off and on it multiple times (I know I was being bad-but I really wanted to know) my take on it is it did nothing for my anxiety ( I also use ativan PRN which really works); however it did pull me out of the lower levels of gloom-but I cannot be certain that was not just a placebo effect-but it was a very distinct effect of the drug. I decided it was not enough of a reason to take it and quit the lexapro altogether.
i think you may be on to something that most people rarely contemplate….and the pharma industry has spent a king’s ransom “nudging” us to believe…….that while highly stressful periods in a person’s life are certainly miserable (and inevitable), people always get better pretty quickly with or without drugs…..a branch of pychology called attribution theory comes into play here……if we take medicine we attribute our “recovery” to medication, making the decision about what to do when the anxiety returns, an easy one. If we call our psychologist for an emergency session’ we attribute the recovery to “a good session with my shrink”. Both explanations are plausible though not likely to be accurate because if you gargled with salt water every morning at 11am for eleven minutes and eleven seconds’ for eleven days your likelihood of “recovery” would also be high; you might then repeat this “remedy” next time things got out of hand for obvious reasons. Human reasoning is by nature a “causive” or associative process and that “association/attribution guides future decisions. But the most likely cause of your recovery is something far less interesting; regression to the mean. Very high states of anxiety represent an extreme condition and extreme conditions,like extreme groups, slide back to the mean over time. This represents an “attribution error” and marketing firms are quite motivated to “nudge” your attribution mechanism in their direction. You were also on the right track with placebo. SSRI (drugs like lexapro) report success rates of .6. Placebo is .3 so that leaves a lot of people thinking that we should be doing a lot better. The anti depressants of a generation ago (tri cyclics) had side effects that were a bit worese for certain patients. Inthe early eighties a new “miracle drug” called prozac became available and i recall their marketing made it seem like SOMA from “Brave New World”. Effectively wiping out tri cyclics like elavil……Can you guess what the success rates and placebos were for these “old fashioned medicines” were? You guessed it.
.6 and .3, respectively..the more things change the more they stay the same.
I recently reduced my dose of Prozac from 40mg to 20 mg, and there is definitely a difference in my anxiety levels! I have learned enough coping mechanisms to deal with it, but if other medical factors did not exist, I would stay on the higher dose. I hate that doctors are so ambivalent about decreasing dosage. Having the responsibility to decide makes me MORE anxious!
I was put in a situation where I would be living abroad for several years and would have to get off meds. It was really the best thing that ever happened to me, because it forced me to find other ways to deal with anxiety. I broke down and ordered Lucinda Bassett’s As-Seen-On-Tv tapes, which opened my mind to the fact that I could detach from the thoughts in my mind.
That gave me some mental preparation for reading Eckhart Tolle’s amazing book “A New Earth.” That got rid of my long-term anxiety and need to be medicated for good. I still have spikes, but once I realize that I’m on the verge of an attack, I know on a deeper level that my mind is either in the past or the future, and if I can just ignore it and be in the present, my anxiety will melt away.
I have suffered, and you know what I mean when I type “suffered,” from anxiety disorder for over 30 years. Ten years ago my psychiatrist who I see just for the twice-yearly med checks, put me on zoloft and ativan, as needed. I do not care if I have to be on these meds for the rest of my life.
My cocktail of choice, as I call the zoloft/ativan prescription, has helped me to enjoy my life the way I should enjoy it. It has not changed my personality. It has not altered my perception of daily life. I am not in a dreamland. I have ups and down days. My cocktail, by inhibiting my anxiety (which I know is clearly hereditary for me), from going to the red zone has helped me be ‘me.’ The real me. The fun me. The empathetic me. The serious me. The real me without the walking on eggshells fear that at anytime I could become paralyzed by my anxiety.
Thank gawd for meds.
Agreed: thank God for meds. It makes me very angry that people assume that one is somehow ‘better’ for leaving meds behind, when going on and off drugs can decrease their efficacy. The whole point of SSRIs and SNRIs is that they affect the brain in meaningful and subtle (and still not well-understood) ways; by contrast, benzodiazepines such as Xanax and Clonapin can be immediately felt, but leave one prey to the underlying symptoms. Benzodiazepines react to existing symptoms; SSRIs and SNRIs, when they are working effectively, remove the symptoms altogether. Thus the fact that we can’t tell that they are working. Who cares if some portion of the effect is placebo? Some portion of it is not. I am so, so grateful that they work, and so, so angry at those who downplay the life-destroying consequences of these illnesses and stigmatize those who get real help. I grew up with a mother who had and still has a major untreated anxiety disorder and depression: my childhood could have been so much richer and happier–and my mother’s life could have been so much richer and happier–if she was not so terrified of the stigma of mental illness that she never sought or received treatment. Right now I’m so angry that if I had a hippie standing in front of me telling me about herbs and meditation, I would punch him in the face with the best right hook I have.
Why don’t you practice Kundalini Yoga? I’m also a very anxious person and, by practicing it, I’ve been able to control it.
This is absolutely terrific, as was the NYTimes piece. The part that is really crippling about being chained to an Rx is when lose your health insurance once the pills are working. Anxiety and depression super escalate when you are asking a pharmacist to sell you one of your SSRI’s, which are $6 each day, so that you can break it in half and not experience too much of the brain shivers of withdrawal while you wait for some kind of medical insurance miracle. The only reason I consider weaning off medication is so that if I ever lack insurance again I won’t have daily breakdowns at Walgreens.
My dad had been on an antidepressant and ativan for many years for anxiety.
When he went into assisted living, for liability reasons ~ older adults are supposedly not supposed to have ativan because they could fall. Well, I never saw a crueler thing happen to a human being with respect to medication in my entire life. Once he was taken off Ativan,
and then put on heavy sedative drugs which he didn’t need, once they wouldn’t give him ativan,
even knowing that he had been on it most of his adult live, he was suffering and never the same.
He died a year later.
Anxiety Disorders are real.
Medication and therapy really do make a quality difference in a person’s life.
Someone ought to lobby to fight the hosptials and the assisted living places,
they ought let the world know what is going on and not, with ativan.
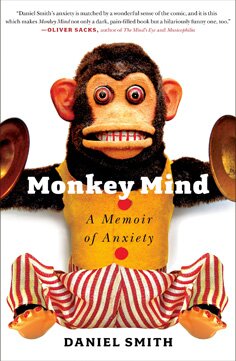
Just finished reading Monkey Mind last night and anticipated writing you a long email (I may anyway, but about other thoughts from the book) about wishing you had spoken more openly about whatever pharmacological tools you have chosen to utilize. My husband is a Ph.D. chemist at one of the largest pharma companies in the U.S. I get SO tired of hearing about conspiracy theories. Ninety-five percent of those scientists truly go to work each morning, hoping to discover something that will make someone’s life a little bit easier. I can say that with all sincerity.